Strategies to Improve Return to Work Outcomes for Employees with PTSD
Jun 26, 2025
Post-traumatic stress injuries, such as PTSD, present complex challenges that can make recovery and workplace reintegration difficult. The longer someone is away from work, the harder it can be to return. Early support to return to work is crucial to increase the likelihood of a successful and sustainable return.
Between 2017 and 2021, nearly 20% of paramedics, 8% per cent of police officers, and 5% of firefighters in Ontario made a compensation claim for a mental health injury related to post-traumatic stress injuries, according to data from the Workplace Safety & Insurance Board (WSIB).1 The Institute for Work and Health (IWH) reports that over 40% of these compensation claims last two or more years2—a concerning trend of extended absences.
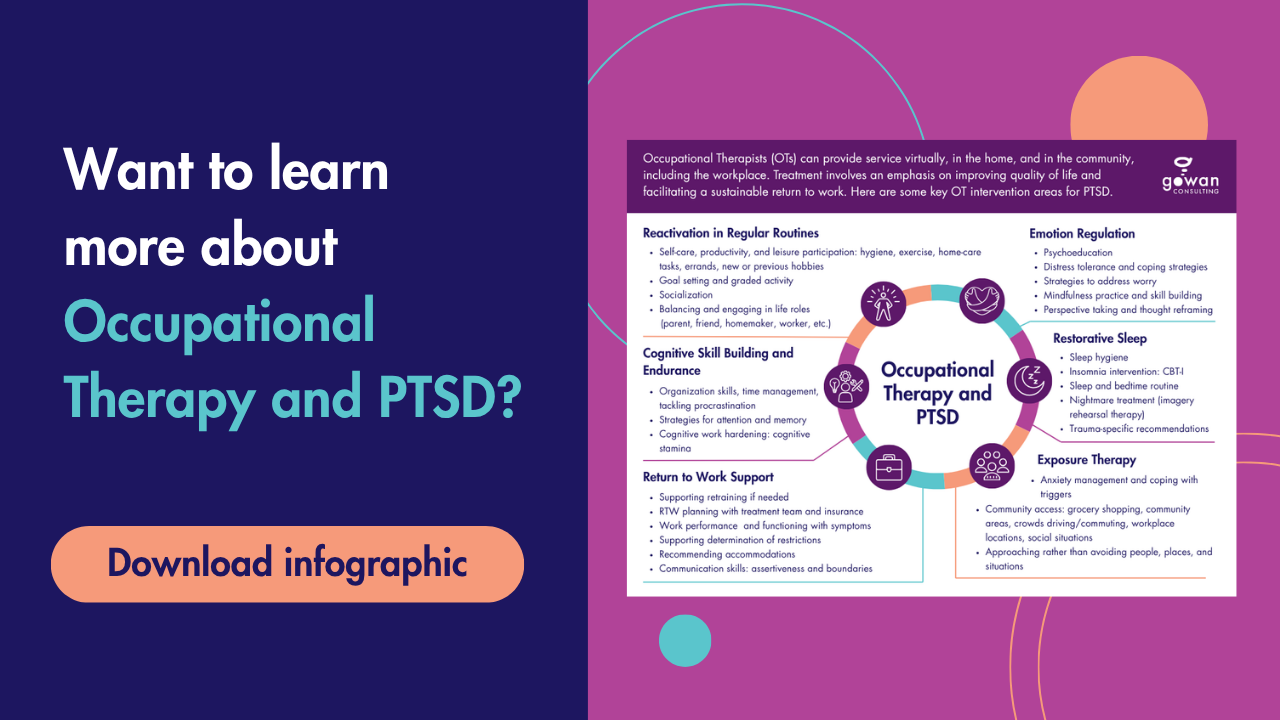
New research from IWH provides insight into the challenges and practices being used by employers to improve recovery and reintegration into the workplace, particularly for those in public service roles. As employers explore innovative solutions, Occupational Therapists (OTs), with their functional and trauma-informed expertise, are uniquely positioned to help move those efforts forward and find creative solutions to improve return to work outcomes.
The Challenge of PTSD in the Workplace
Post-traumatic stress injuries are one of the most complex health challenges in occupational rehabilitation. The symptoms, work limitations, and triggers can vary widely person to person. Cognitive impairments that affect decision-making, emotional regulation, and environmental sensitivities can surface in unique ways depending on the workplace, nature of the trauma, and the individual. Some symptoms and limitations may only become apparent when workers attempt to return to their pre-injury roles.
This unpredictability creates significant challenges for employers attempting to develop appropriate accommodations. Additionally, the effects of PTSD are often long-lasting, requiring long-term management strategies rather than temporary accommodations. Not every individual will heal and be able to perform regular duties within the same timeline. Therefore, return to work plans must be personalized, flexible, and responsive to evolving recovery needs.
Common Organizational Barriers
When faced with the challenge of PTSD, organizations may not have the tools or processes in place to effectively support employees. Barriers may include:
- Resource and Expertise Gaps: Many organizations do not have trained disability managers or mental health professionals to effectively manage PTSD-related disability claims. HR teams may be left to handle complex cases without the appropriate background. Some external healthcare providers may also lack the specialized knowledge needed about public safety roles, leading to suboptimal return-to-work outcomes.
- Limited Accommodation Options: The size and nature of an organization directly affects its ability to provide meaningful work accommodations. Smaller organizations have fewer alternative roles available, while certain professions have inherently limited options for modified duties. This can leave employees with few viable pathways back to work within their skill set and organization.
- Stigma and Cultural Barriers: Persistent stigma surrounding mental health can delay disclosure and support. Employees may fear being judged, supervisors may lack training on accommodations, and organizational culture may discourage open conversations about psychological wellness. A lack of trust between employee and employer breaks down communication and the ability to provide proactive support.
Innovative Employer Strategies and the Role of OTs
To overcome the barriers, employers are implementing innovative strategies to improve return to work outcomes. OTs can play a key role in designing, facilitating, and supporting these approaches. Because of their combination of clinical expertise and focus on function in the workplace, OTs are the ideal partners for PTSD return-to-work initiatives.
Proactive Mental Health Management and Early Intervention
Some organizations are shifting from reactive approaches to proactive mental health management—using regular check-ins, attendance monitoring, preventive time off after critical incidents, and documentation of potential trauma exposure. These strategies support early detection and intervention. OTs can contribute to this strategy by collaborating with stakeholders to design evidence-based prevention programs, accommodation policies, and reintegration protocols.
Another key part of this approach is training for staff to recognize early signs of distress and how to respond supportively. This lays the groundwork for a culture where workers feel safe to disclose and seek help. OTs are great resources for team education on mental health awareness, peer and leadership support, stigma, psychological safety, and accommodations.
Dedicated Mental Health Support
Employers are investing in internal wellness teams, peer support programs, and specialized disability case management roles to create ongoing, reliable support for workers experiencing PTSD. OTs can work closely with these internal teams by offering functional expertise that can fill gaps in return to work and accommodation planning.
Most mental health professionals are trained to address psychological symptoms, but not necessarily how those symptoms affect work tasks, productivity, or occupational functioning. OTs specialize in connecting mental health challenges to real-world work demands. Conducting treatment in actual work environments is an important part of their method. Their specialized knowledge in trauma-informed care, public safety roles and culture, and complex case management makes them the perfect ally to help address the “work” part of mental health at work.
Collaborative Return-to-Work Models
The most successful return to work (RTW) programs involve phased reintegration, living RTW plans that evolve over time, and consistent involvement from employers, healthcare providers, and case managers. These collaborative approaches support sustainable reintegration and reduce the risk of re-injury at work.
OTs are ideally positioned to lead and coordinate these models. They create individualized, graduated RTW plans, provide job coaching, and offer real time support to adjust pace and duties to align with employee recovery. As part of multi-stakeholder teams, OTs can facilitate alignment, manage expectations, and ensure consistency throughout the RTW process, acting as the linking agent to build trust between all parties and keep communication flowing.
Functional Job Matching and Flexible Accommodation Design
Traditional disability assessments often fail to capture the nuanced functional impacts of PTSD, leading to vague or highly restrictive restrictions such as "no inmate contact." Forward-thinking employers are moving beyond generic job descriptions to understand the real demands of each role. By understanding a job’s core tasks, they can identify more flexible placement and accommodation opportunities that align with a worker’s current capabilities.
OTs play a central role in this process through detailed, task-based job analyses and comprehensive functional assessments. By evaluating the physical, cognitive, and emotional demands of work and assessing environmental stressors, OTs can identify trauma-informed accommodations that target employees’ unique needs and promote long-term success.
How to Access Support for Return to Work
Employees and organizations don’t need to face the complexities of PTSD-related return to work alone. Occupational Therapists offer valuable support that complements the work of internal wellness teams, HR professionals, and external mental health providers.
Employees may be referred to an OT through their employer’s disability management program, extended health benefits, or a workers’ compensation claim. Healthcare providers and case managers can also refer individuals to Occupational Therapy when PTSD symptoms are affecting work participation.
If you’re an employee experiencing a post-traumatic stress injury, you can ask your healthcare team, employer, or insurer if OT services are covered or available as part of your recovery and reintegration plan. Contact Gowan Consulting to get matched with an Occupational Therapist.
If you’re an employer considering your options for proactive workplace support, contact Gowan Consulting for guidance on program development and staff training.
If you’re an HR or Disability Manager with a complex PTSD case, request a functional assessment and return to work planning support by making a referral to Gowan Consulting.
Resources
[1] Institute for Work & Health. Employers face challenges in supporting public safety personnel with post-traumatic stress injuries. (2025, January). https://www.iwh.on.ca/plain-language-summaries/employers-face-challenges-in-supporting-public-safety-personnel-with-post-traumatic-stress-injuries
[2] Institute for Work & Health. How employers are improving RTW outcomes for public safety workers with PTSI. (2025, March). https://www.iwh.on.ca/news/how-employers-are-improving-rtw-outcomes-for-public-safety-workers-with-psti